Categories
 Buy Adderall Online
Buy Adderall Online
 Buy Adipex Online
Buy Adipex Online
 Buy Alprazolam Online
Buy Alprazolam Online
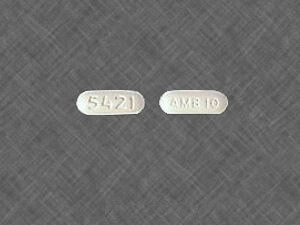 Buy Ambien Online
Buy Ambien Online
 Buy Ativan Online
Buy Ativan Online
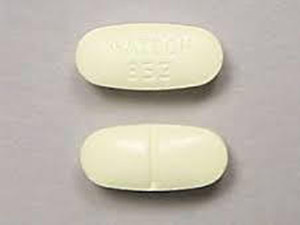
 Buy Carisoprodol Online
Buy Carisoprodol Online
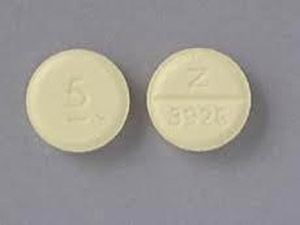
 Buy Clonazepam Online
Buy Clonazepam Online
 Buy Codeine Online
Buy Codeine Online
 Buy Darvocet Online
Buy Darvocet Online
 Buy Demerol Online
Buy Demerol Online
 Buy Diazepam Online
Buy Diazepam Online
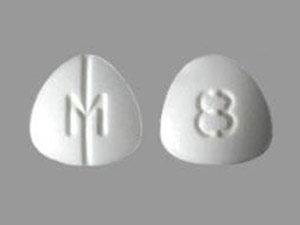
 Buy Dilaudid Online
Buy Dilaudid Online
 Buy Fioricet online
Buy Fioricet online
 Buy Gabapentin Online
Buy Gabapentin Online
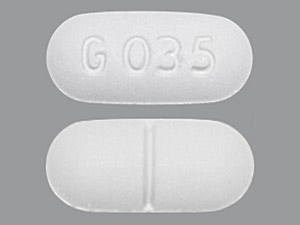
 Buy Hydrocodone Online
Buy Hydrocodone Online
 Buy Hydromorphone Online
Buy Hydromorphone Online
 Buy Klonopin Online
Buy Klonopin Online
 Buy Lexapro Online
Buy Lexapro Online
 Buy Lorazepam Online
Buy Lorazepam Online
 Buy Lorcet Online
Buy Lorcet Online
 Buy Lortab Online
Buy Lortab Online
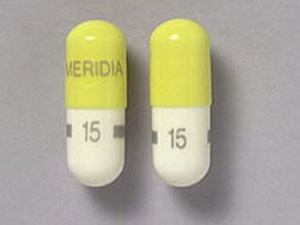 Buy Meridia Online
Buy Meridia Online
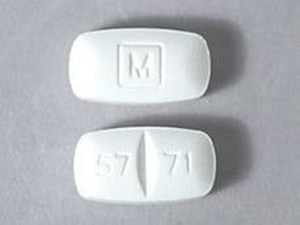 Buy Methadone Online
Buy Methadone Online
 Buy Modafinil Online
Buy Modafinil Online
 Buy Norco Online
Buy Norco Online
 Buy Opana ER Online
Buy Opana ER Online
 Buy Oxycodone Online
Buy Oxycodone Online
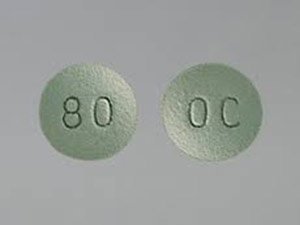 Buy Oxycontin Online
Buy Oxycontin Online
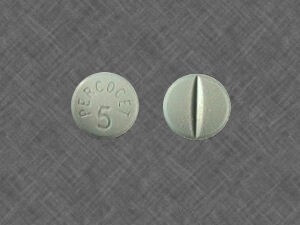 Buy Percocet Online
Buy Percocet Online
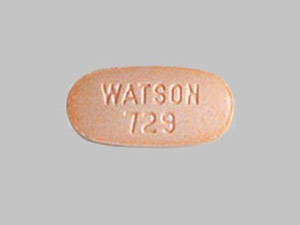
 Buy Phentermine Online
Buy Phentermine Online
 Buy Roxicodone Online
Buy Roxicodone Online
 Buy Soma Online
Buy Soma Online
 Buy Suboxone Online
Buy Suboxone Online
 Buy Subutex Online
Buy Subutex Online
 Buy Tapentadol Online
Buy Tapentadol Online
 Buy Tramadol Online
Buy Tramadol Online
 Buy Valium Online
Buy Valium Online
 Buy Viagra Online
Buy Viagra Online
 Buy Vicodin Online
Buy Vicodin Online
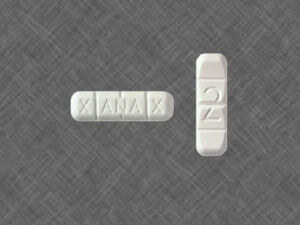 Buy Xanax Online
Buy Xanax Online
 Buy Zolpidem Online
Buy Zolpidem Online

Products
-
 Tapentadol 100mg
Rated 5.00 out of 5$350.00
Tapentadol 100mg
Rated 5.00 out of 5$350.00 -
 Modafinil 200mg
Rated 5.00 out of 5$369.00
Modafinil 200mg
Rated 5.00 out of 5$369.00 -
 Modafinil 100mg
Rated 5.00 out of 5$349.00
Modafinil 100mg
Rated 5.00 out of 5$349.00 -
 Klonopin 2mg
Rated 5.00 out of 5$339.00
Klonopin 2mg
Rated 5.00 out of 5$339.00 -
 Klonopin 1mg
Rated 5.00 out of 5$329.00
Klonopin 1mg
Rated 5.00 out of 5$329.00
Recent Posts
- Relief From Kidney Stone Pain – Effective Strategies And Solution
- Best Nerve Pain Medication for the Elderly
- Sleep habits and their effects on human brain activity
- Does drinking more water help you lose weight?
- Alprazolam for anxiety benefits and risk
- Tramadol vs Dilaudid – Which is the best for severe pain
- How Long Does Hydromorphone Stay in Your System?
- How to spot fake Xanax (alprazolam) pills
- Does Suboxone help with pain?
- How to know if green Xanax s 90 3 pill is fake?

Scientists, policymakers, and healthcare workers are keen to ascertain to what extent COVID-19 may be seasonal. By understanding this aspect of the disease, we could guide our response to the pandemic.
UC Santa Barbara’s researchers have found evidence that the spread of COVID-19 is sensitive to UV exposure. In contrast, this suggests that COVID-19 may vary with the seasons, other seasonal factors such as temperature, specific humidity, and precipitation—whose effects are uncertain according to the available data. The results came in the Proceedings of the National Academy of Sciences.
According to co-author Kyle Meng, “Resembling species of coronavirus such as SARS from 2003 and MERS from 2012, turned out to have weak relationships with temperature and humidity, but were sensitive to UV radiation”. Kyle Meng is an environmental economist in UC Santa Barbara’s economics department and at the campus’s Bren School of Environmental Science & Management.
Meng, in collaboration with Tamma Carleton, also at the Bren School, Peter Huybers and Jonathan Proctor from Harvard, and Jules Cornetet at France’s École Normale Supérieure Paris-Saclay, sought to explore the relationship between UV radiation and the spread of COVID-19 by creating a high-resolution global dataset of daily COVID-19 cases.
Many papers compare various locations to get a sense of how the disease reacts to different environmental conditions. But this approach presents a host of potentially confounding factors into statistical models, such as health care quality, income, and cultural norms.
Meng extends the more temperate United States and more tropical Brazil as models. He said, “The U.S. and Brazil differ for a lot of reasons. They differ in economic conditions and institutions, in addition to different environmental conditions.” He said these distinctions prevent a clean comparison of the spread of COVID-19 based solely on environmental conditions.
To overcome this problem, the team carried out a longitudinal study, essentially comparing many populations to themselves over time. So, rather than comparing Brazil to the U.S., they compared communities within Brazil to themselves at a different time, when local environmental conditions changed. “We investigate whether daily fluctuations in environmental conditions experienced by a population affect new COVID-19 cases up to two weeks later,” Meng described.
To achieve this, the researchers required bulk of data. Unfortunately, when the team started their research, international COVID-19 databases, like that of Johns Hopkins, provided data only at the country level. Records with more satisfactory resolution were available across different agencies and institutions in various languages and formats.
“We utilized many diverse datasets from different countries’ statistical agencies and synchronized them to form a global dataset comprised of over 3,000 spatial units,” Carleton said. The authors then employed a dataset of meteorological conditions with a daily resolution to match local environmental circumstances to daily counts of COVID-19 cases.
The researchers employed a set of statistical techniques to analyze how four variables viz. UV radiation, temperature, humidity, and precipitation—correlated with the daily growth rate of COVID-19 cases, a measure for how rapidly the disease was spreading in a region. They also evaluated the lag time between changes in environmental conditions and possible effects on recorded COVID cases, which could be significant given the virus’s 4 to 7 day incubation period, along with additional testing delays.
The team manifested that a location’s UV exposure profoundly affects COVID-19 transmission. A shift in UV exposure by one standard deviation (approximately equal to the difference in UV between May and June in Los Angeles) diminished the growth rate of new cases by around one percentage point over the following two weeks. It means that it could bring down COVID-19 growth rates from an average daily increase at the beginning of the epidemic of 13% to a 12% increase per day.
Based on the expected UV radiation’s seasonal changes, the model predicted growth rates would increase by 7.3 percentage points for southern temperate locations between January and June. While, northern temperate regions would see a UV-driven decrease of 7.4 percentage points during that same period, as longer days increased UV exposure.
This pattern shifts as the seasons change. By December, the researchers predicted COVID-19 growth rates could decline by around 7.7 percentage points in southern temperate zones, with July numbers, while cooler northern areas could see an inflation of 7.8 percentage points over this period.
Notably, the seasonal influence of UV on the transmission of the disease is small compared to that of social distancing policies such as travel restrictions, school closures, or home isolation, the authors noted. Regardless of the weather, social distancing measures appear to be necessary to slow the spread substantially.
The infection rates appear to have decreased in the northern hemisphere during the summer, possibly due to increased UV exposure, which confirms these findings. However, many regions also relaxed their COVID stay-at-home orders simultaneously, Meng said. Due to this, there’s a conflation between UV effects and easing the restrictions during the summer months. “This is a huge reason why our study utilizes daily fluctuations in UV exposure to avoid conflating influencing factors when studying long-term, varying fluctuations.”
The U.S. is currently experiencing a rise in COVID-19 infections with winter’s arrival, and these findings are consistent with these concerns. According to Carleton, “We are confident of the UV effect, but this is only one piece of the full seasonality picture.”
Lab studies will eventually be crucial in exploring the mechanisms at work. However, the authors suspect multiple factors may be behind UV’s effect on COVID-19 transmission, some of which are difficult to study in the lab- the first one is biological. UV can damage the nucleic acids that the virus utilizes to encode its genetic information. Co-author Jonathan Proctor, a post-doctoral fellow at Harvard, posited that UV radiation might inactivate the virus as transmitted, such as when it’s suspended in the air or resting on an exposed surface. “Just as UV can destroy our DNA if we don’t use sunscreen, UV can damage the COVID-19 virus,” Proctor said.
Another component is behavioral. For instance, people may go out more often when it is more sunshiny, altering transmission risk. While laboratory studies are useful in determining biological mechanisms, population-level studies like this can also consider social factors.
“In this context, our study suggests that seasonal changes in UV may affect COVID-19 transmission in the months to follow,” Meng said. “And if that’s true, we need to contemplate ways of modulating COVID-19 containment policies seasonally.”
Written by admin
Coupon Code
Use Coupon CodeSALE10
Product Categories
- Buy Adderall Online
- Buy Adipex Online
- Buy Alprazolam Online
- Buy Ambien Online
- Buy Ativan Online
- Buy Carisoprodol Online
- Buy Clonazepam Online
- Buy Codeine Online
- Buy Darvocet Online
- Buy Demerol Online
- Buy Diazepam Online
- Buy Dilaudid Online
- Buy Fioricet online
- Buy Gabapentin Online
- Buy Hydrocodone Online
- Buy Hydromorphone Online
- Buy Klonopin Online
- Buy Lexapro Online
- Buy Lorazepam Online
- Buy Lorcet Online
- Buy Lortab Online
- Buy Meridia Online
- Buy Methadone Online
- Buy Modafinil Online
- Buy Norco Online
- Buy Opana ER Online
- Buy Oxycodone Online
- Buy Oxycontin Online
- Buy Percocet Online
- Buy Phentermine Online
- Buy Roxicodone Online
- Buy Soma Online
- Buy Suboxone Online
- Buy Subutex Online
- Buy Tapentadol Online
- Buy Tramadol Online
- Buy Valium Online
- Buy Viagra Online
- Buy Vicodin Online
- Buy Xanax Online
- Buy Zolpidem Online

Leave a Reply